Many individuals who experience substance use disorders and could benefit from treatment do not receive care.
According to SAMHSA’s National Survey on Drug Use and Health (NSDUH)1, in 2017, an estimated 20.7 million (or 1 in 13) people age 12 and over needed treatment for a substance use disorder. However, only 4 million age 12 and over received any substance use treatment that year -- less than 20% of the population who needed it.
In other words: in 2017, only about 80% of Americans who needed treatment didn't receive it (16.7 million).
According to NSDUH, the two most common reasons given by people age 12 and over who felt they needed treatment but did not receive it, were:
- They were not ready to stop using alcohol or illicit drugs (39.7%), or
- They had no health care coverage and could not afford the cost of treatment (30.3%%).
Similarly, among all adults and among adults with any mental illness or among those with severe mental illness who perceived a need for mental health services but did not receive them, inability to afford the cost of care was the most commonly reported reason for not receiving services.
Removing Barriers Improves Retention
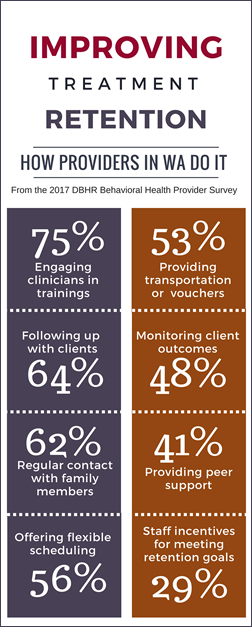
Providers in Washington State surveyed as part of the 2017 Behavioral Health Provider Survey noted a range of approaches used to improve retention both in treatment and during client transition to another level of care.
The most common ways providers try to improve retention outcomes are featured in the infographic on the right (view a larger version here). In addition to those 8 techniques, providers also reported using co-location of other services (27%), participation incentives/contingency management for clients (22%), use of child and family teams (20%), linking clients with a sponsor (12%), and on-site child care (6%).
The most common approaches Washington providers use to achieve client transition to another level of care are:
- Obtain client signature on consent forms to clinicians can exhange information (87%)
- Establish phone/fax contact with the other level of care setting regarding the client (77%)
- Talking with the case manager (74%)
- Calling the other level of care location to alert them that the client is coming (66%) and to send them the client's file (48%).
Some Advice from NIATx
 Have regular conversations with clients about barriers to staying in treatment may help them solve problems and continue when personal or family issues arise.
Have regular conversations with clients about barriers to staying in treatment may help them solve problems and continue when personal or family issues arise.- Help clients anticipate and solve logistical problems involved with starting and staying in treatment, including: transportation, childcare, ability to pay, translation needs, other appointments, the criminal justice system, and work schedules.
Two success stories (from NIATx)
 The Partnership for Advancing Recovery in Kentucky installed webcams in agencies that worked together so that clients would meet a counselor in the outpatient program before leaving residential treatment. They also arranged for doctors to use video conferencing to meet with clients who lived in rural areas. For more information about this change and other changes implemented by PARK, see the PARK Continuum of Care.
The Partnership for Advancing Recovery in Kentucky installed webcams in agencies that worked together so that clients would meet a counselor in the outpatient program before leaving residential treatment. They also arranged for doctors to use video conferencing to meet with clients who lived in rural areas. For more information about this change and other changes implemented by PARK, see the PARK Continuum of Care.
 The Center for Human Services in Seattle, WA decreased no-show rates from 80% to 65% and increased admissions by 87% by performing assessments at the Community Service Office (the referrer) one day a week instead of requiring all assessments be done at their facility. For more information, see the CHS story (on the NIATx site).
The Center for Human Services in Seattle, WA decreased no-show rates from 80% to 65% and increased admissions by 87% by performing assessments at the Community Service Office (the referrer) one day a week instead of requiring all assessments be done at their facility. For more information, see the CHS story (on the NIATx site).
Resources
 NIATx Resources on Eliminating Barriers to Treatment
NIATx Resources on Eliminating Barriers to Treatment
Includes stories about successful implementation at real treatment agencies, lessons learned, tracking measures, action steps, and more.
Community Health Centers and First Responders: Strengthening Communities through Education
Webcast addresses the behavioral health needs relevant for rural and frontier communities, share innovative approaches to addressing them in remote areas, and review the challenges faced when attempting to reduce the treatment gap for rural and frontier residents. It also addresses special considerations of Native American/American Indian communities living in rural areas.
Recovery Among Diverse Populations
 Webcase explores best practices and methods for overcoming barriers to connect clients with culturally responsive treatment and recovery services.
Webcase explores best practices and methods for overcoming barriers to connect clients with culturally responsive treatment and recovery services.
TAP 33: Systems-Level Implementation of Screening, Brief Intervention, and Referral to Treatment (SBIRT)
SAMHSA Technical Assistance Publication Series manual about SBIRT services implementation, covering challenges, barriers, cost, and sustainability.
NAADAC Webinar: Improving Retention and Outcomes: The Partners for Change Outcome Management System (2015)
Learn what is being used effectively with clients across behavioral health diagnostic categories and in public and private service delivery systems resulting in significantly reduced dropouts and improved recovery outcomes.
Webinar: Treatment 101: Finding Effective Care
Recovery Month Webcast, April 2018, Panelists also address the barriers to quality care, treatment of co-occurring disorders, and the role behavioral health counselors can play in primary care settings.
References & Readings
- Substance Abuse and Mental Health Services Administration. Key Susbsance Use and Mental Health Indicators in the United States: Results from the 2017 National Survey on Drug Use and Health. September 2018. [free online]